Vasectomy and Testicular Macrophage Reprogramming
Introduction
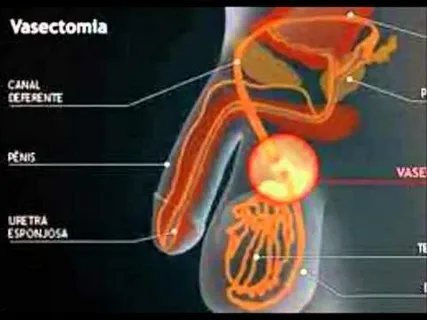
Vasectomy is a widely utilized surgical procedure for male sterilization, offering a permanent and reliable method of birth control. The technique involves cutting or sealing the vas deferens, thereby preventing sperm from mixing with semen. While it is typically considered a safe and localized intervention, emerging studies in immunology and testicular biology reveal deeper systemic effects, particularly concerning immune cells in the testis. One area of growing interest is how vasectomy may influence the activity and identity of testicular macrophages—specialized immune cells essential for maintaining immunological tolerance and supporting spermatogenesis.
Testicular macrophages play a unique and dual role: they regulate inflammation and participate in tissue repair, while also maintaining the immune-privileged environment required for sperm cell development. This article explores how vasectomy alters the phenotypic and functional programming of testicular macrophages, potentially influencing testicular homeostasis, fertility reversibility, and immune responses within the male reproductive tract.
Understanding Testicular Macrophages
Macrophages are a diverse population of immune cells derived from monocytes. In the testis, they are mainly located in two regions: interstitial macrophages, found in the interstitial space near Leydig cells, and peritubular macrophages, which are closer to the seminiferous tubules. Their roles include:
- Maintaining immune privilege by suppressing autoimmunity against sperm antigens.
- Modulating inflammation after infection or tissue injury.
- Assisting spermatogonial stem cell (SSC) maintenance through cytokine release and interaction with Sertoli cells.
- Supporting steroidogenesis in collaboration with Leydig cells.
Testicular macrophages exhibit a specialized phenotype different from their counterparts in other organs. They tend to express anti-inflammatory markers (such as CD206) and secrete immunoregulatory cytokines like IL-10 and TGF-β.
The Immune Landscape Before and After Vasectomy
Pre-vasectomy, the testis is an immune-privileged site, in part due to the blood-testis barrier (BTB) and regulatory macrophage activity. This immunological barrier protects developing germ cells, which appear postnatally and could otherwise be recognized as foreign by the immune system.
Following vasectomy, immune privilege may be disrupted. The key events include:
- Breakdown of epithelial barriers due to pressure buildup or backflow of sperm.
- Sperm granuloma formation, a localized immune response to leaked sperm antigens.
- Antisperm antibody (ASA) production, a sign of autoimmune sensitization.
Within this changing landscape, testicular macrophages are reprogrammed—both functionally and transcriptionally—toward phenotypes more aligned with classical (M1) or mixed inflammatory profiles.
Macrophage Reprogramming After Vasectomy
Macrophage polarization is often conceptualized along an M1-M2 spectrum:
- M1 macrophages: Pro-inflammatory, express TNF-α, IL-6, inducible nitric oxide synthase (iNOS).
- M2 macrophages: Anti-inflammatory, express IL-10, CD163, and promote tissue repair.
Following vasectomy, testicular macrophages begin to shift toward an M1-like phenotype, particularly near granulomatous regions and vasal rupture sites. This reprogramming is driven by:
- Exposure to sperm antigens: Macrophages encounter previously sequestered sperm proteins, triggering immune activation.
- Tissue injury: The surgical trauma itself promotes a pro-inflammatory wound healing response.
- Cytokine milieu changes: Increased levels of IFN-γ and IL-1β can skew macrophages toward inflammatory roles.
This functional shift compromises their immune-regulatory role and alters local cytokine networks, potentially impairing spermatogenesis, even in regions distant from the surgical site.
Epigenetic and Transcriptomic Changes
Recent transcriptomic analyses using single-cell RNA sequencing (scRNA-seq) have revealed that vasectomy induces distinct transcriptional profiles in testicular macrophages. These include:
- Upregulation of TLR signaling pathways, indicating increased sensitivity to pathogen- or damage-associated molecular patterns.
- Downregulation of immunosuppressive genes such as Arg1 and IL-10.
- Altered expression of chemokines like CCL2 and CXCL10, which can recruit other immune cells and escalate inflammation.
In addition to transcriptional changes, epigenetic remodeling—including histone modifications and altered DNA methylation—has been observed in macrophages post-vasectomy. These changes contribute to a sustained inflammatory phenotype, potentially impacting long-term testicular health.
Impact on Testicular Function and Fertility Reversal
One of the lingering questions surrounding vasectomy is its reversibility. Although vasovasostomy (reversal surgery) can reestablish the physical continuity of the vas deferens, restored fertility is not guaranteed. One possible explanation is the immune-mediated damage to testicular tissue caused by reprogrammed macrophages.
Pro-inflammatory macrophages may:
- Promote fibrosis in the epididymis or vas deferens.
- Inhibit Leydig cell steroidogenesis, reducing testosterone levels.
- Disrupt the stem cell niche required for effective spermatogenesis.
This underscores the importance of understanding and potentially modulating macrophage responses in the context of vasectomy and its long-term consequences.
Animal Models and Evidence
Rodent models, particularly in rats and mice, have been instrumental in uncovering the role of macrophage reprogramming post-vasectomy. In these models:
- Macrophage infiltration increases in the epididymis and testis within days after vasectomy.
- F4/80+ macrophages exhibit elevated MHC-II expression, consistent with antigen presentation activity.
- Knockout models for IL-10 or TGF-β show exaggerated inflammatory responses and granuloma formation after vasectomy.
These models support the hypothesis that testicular macrophages undergo profound reprogramming, leading to tissue changes not solely attributable to mechanical obstruction or sperm leakage.
Clinical Relevance and Human Implications
In humans, while most vasectomy patients do not experience long-term complications, a minority report post-vasectomy pain syndrome (PVPS), chronic testicular discomfort, or altered hormone levels. These symptoms may reflect persistent low-grade inflammation or immune activation.
Histopathological studies of testicular biopsies post-vasectomy show increased presence of CD68+ macrophages, often near degenerating seminiferous tubules. Inflammatory cytokines such as IL-1β and TNF-α are elevated in seminal plasma post-vasectomy in some individuals.
This raises the possibility of targeting macrophage pathways for therapeutic interventions, such as:
- Use of anti-inflammatory agents post-operatively to preserve testicular immune privilege.
- Exploring macrophage reprogramming drugs (e.g., IL-10 mimetics or TLR inhibitors) to prevent chronic inflammation.
- Personalized counseling about immune-related risks for patients considering vasectomy.
Research Gaps and Future Directions
Despite advances, several critical questions remain:
- What are the longitudinal effects of macrophage reprogramming on testicular function over decades?
- Can macrophage phenotypes be reversed pharmacologically after vasectomy?
- Are there genetic predispositions that make certain individuals more prone to inflammation or PVPS post-vasectomy?
Addressing these questions requires integrated research spanning immunology, reproductive biology, and urology, especially in translating findings from animal models to human clinical practice.
Conclusion
Vasectomy, while effective and safe in most cases, initiates complex immunological changes within the testicular microenvironment. Chief among these is the reprogramming of testicular macrophages, shifting from an immune-tolerant state to one of inflammation and antigen presentation. This transformation may have broader consequences for fertility, testicular health, and postoperative complications.
Understanding the intricate dynamics of macrophage phenotypes opens new doors for improving vasectomy outcomes and addressing long-term risks. As research deepens, therapeutic targeting of immune pathways may evolve into a novel strategy for enhancing male reproductive care.
FAQs
Q1: Does vasectomy affect immune cells in the testis?
Yes. After vasectomy, testicular macrophages may shift from a regulatory to an inflammatory phenotype. This reprogramming can influence tissue integrity, immune responses, and spermatogenic support.
Q2: Can the effects of macrophage reprogramming after vasectomy be reversed?
Potentially. While research is still evolving, anti-inflammatory therapies or immune-modulatory drugs may reverse or mitigate some effects of macrophage reprogramming, especially if administered early.
Q3: Is macrophage reprogramming responsible for post-vasectomy pain?
It may play a role. Chronic inflammation driven by reprogrammed macrophages could contribute to post-vasectomy pain syndrome (PVPS), although other factors like nerve injury and fibrosis are also involved.


